Mastering the Art of Panic Attack Prevention: From Panic to Peace

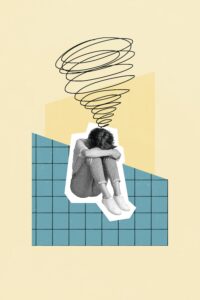
In the labyrinth of life, there are moments when the body’s fight-or-flight response becomes triggered with astounding intensity out of the blue, despite there being no imminent danger around us. These moments are referred to as “panic attacks.”
Whether you’re someone who personally experiences panic attacks or you’re hoping to support a loved one, these tips can help you navigate the storm that is panic attacks.
Symptoms of a Panic Attack
Many times, panic attacks are physical manifestations one experiences as a result of high anxiety levels. These physical symptoms can be so severe an individual experiencing them may believe they are having a heart attack. Panic attacks can be triggered by severe anxiety, phobias, a change in environment or by being under heavy, long-term stress.
Signs you may be having a panic attack include:
- Hyperventilation (rapid breathing)
- Rapid heartbeat
- Sudden numbness in the hands
- Nausea
- Chest pain that feels “stuck” in the mid-chest area
- Sudden dizziness
- Hot flashes
- Shortness of breath (feeling like you can’t get enough air)
- Shivering or shaking uncontrollably
- “Pins and needles” sensation (the feeling of uncomfortable tingling or prickling)
While it’s hard to stop a panic attack in its tracks, there are ways you can regain control, lessen the intensity of symptoms and ease yourself out of this uncomfortable experience.
How to Work Through a Panic Attack
Sensory grounding
- The keywords here are ice and sweets. If you’re able to, grab a cold washcloth, water bottle or ice cube and rub it on your face. Panic attacks can induce hot flashes so cold stimuli may help you to cool down and calm down, which in turn can shorten panic attacks and make them more bearable. Another way to try this type of sensory grounding is to quickly dunk your head or face under cold water (make sure the water isn’t too freezing first!). Some people prefer to do the “sour candy trick” instead by sucking on a super sour candy when feeling panicked. The tart taste helps with refocusing and shifting attention away from the symptoms of a panic attack. If you’re prone to panic attacks, we recommend carrying sour candy around whenever you’re out and about so you always have them handy, just in case.
Affirmation statements
- Work on telling yourself positive, affirmative statements. These can be phrases like “This will pass and is temporary,” “I am in control, I’m feeling overwhelmed but I will get through this,” or “This feeling is uncomfortable but not dangerous.”
Close your eyes + do square breathing
- Closing your eyes may help you calm down and block out overstimulation around you in order to bring you back to the present. While your eyes are closed, practice the “square” breathing technique, also referred to as “box breathing.” This technique happens in fours. Begin by letting trapped air out through your mouth, then inhale through your nose for four seconds. Hold that breath for another four, then exhale to the count of four.
Adopt a “focus object”
- It can be helpful to adopt a focus object, which is something around you to focus all of your attention on during a panic attack. When you decide on an object, try and take mental notes of everything about it. This can include the texture, color, shape, sound, temperature or smell of your chosen object. This method is useful for both relaxing and distracting your brain from panic attack symptoms.
What Can I Do to Prevent Panic Attacks?
- Practice mindfulness. Practice mindfulness regularly by saying daily affirmations or taking five minutes each morning to practice deep breathing.
- Keep an orange in the freezer. Though it may sound odd, having a frozen orange on hand can help when you are experiencing high anxiety or feel a panic attack coming on. When you start to notice the onset of panic attack symptoms, grab the frozen orange and rub it on your neck, arms or face. The freezing cold sensation of the orange as well as its bumpy texture can essentially “shock” an overwhelmed sympathetic nervous system back to its neutral and relaxed state.
- Take preventative lifestyle measures. If you do feel relatively more anxious than normal, it could be beneficial to cut out or cut down on things that have been shown to increase anxiety, such as caffeine, cigarettes and alcohol.
- Prioritizing getting enough sleep. Sleep is crucial in times when we experience severe anxiety. When you’re sleep deprived, this prompts a higher level of cortisol through the bloodstream, which in turn activates the nervous system and puts us at a higher risk of experiencing physiological symptoms of anxiety—like panic attacks.

What Should I Do After Having a Panic Attack?
Following a panic attack, many individuals still experience lingering physical and emotional pain and anxiety, sometimes referred to as a “panic attack hangover.” After a panic attack, we’re often left feeling exhausted and completely fatigued. It’s easy to feel mentally trapped and stuck in a state of still feeling panicked or on overdrive, even after the panic attack itself has ended.
When you catch yourself caught up in the dread of a panic attack hangover, remember that there are ways to get you out of this funk that don’t require much energy.
First, try journaling. Journaling is a great and easy way to get all your thoughts down on paper and focus on being present in the moment. Not only will this help relieve some anxiety, but it will also allow you to clear your head and focus better afterwards.
Exercise—like meditation, yoga, or walking—is another great way to refocus your energy and mind, allowing you to get yourself into a new environment.
Getting a good night’s rest and fueling yourself with nutritious food can also help curb a panic attack hangover by boosting energy and reducing fatigue. Learning how to manage panic attacks can be a long and hard process, but worthwhile in the end. Continue to be patient with yourself and give yourself grace while exploring new techniques that work for you. With time and effort, you can gain control over your panic attacks.
Additional Support
Therapists and psychiatrists are a great resource for anyone who struggles with anxiety. Valera Health’s licensed medical professionals are here to provide you with additional anxiety support should you need it. If you’d like to work with a therapist or psychiatrist who can help you manage your anxiety, visit www.valerahealth.com/consult-today/ or click here to schedule a free consultation with a dedicated Health Connector.

Works Referenced:
American Psychological Association. (n.d.). Panic disorder: Answers to your most important questions . American Psychological Association. https://www.apa.org/topics/anxiety/panic-disorder
Brognano, W. by: A. (n.d.). Panic (anxiety) attack hangover: Symptoms & how to cope. Choosing Therapy. https://www.choosingtherapy.com/panic-attack-hangover/
Gotter, A. (2023, February 28). 11 ways to stop a panic attack. Healthline. https://www.healthline.com/health/how-to-stop-a-panic-attack#prevention
Group, P. (n.d.). What to do when you feel the signs of a panic attack coming on. https://www.priorygroup.com/blog/what-to-do-when-you-feel-the-signs-of-a-panic-attack-coming-on
Marks, J. (2021, October 8). The best grounding techniques for anxiety relief. Psych Central. https://psychcentral.com/anxiety/using-the-five-senses-for-anxiety-relief
Pallarito, K. (2022, June 9). 14 signs you’re having a panic attack. Health. https://www.health.com/condition/anxiety/panic-attack-symptoms
Perkins, C. (2021, August 4). The science behind panic attacks – and what you can do to manage them. ideas.ted.com. https://ideas.ted.com/the-science-behind-panic-attacks-and-what-can-you-do-to-manage-them/
Person. (2021, October 19). Do candy warheads stop panic attacks? 5 panic attack hacks that work. Nebraska Medicine. https://www.nebraskamed.com/behavioral-health/do-candy-warheads-stop-panic-attacks-5-panic-attack-hacks-that-work
Schuckit, M. A. (1996). Alcohol, anxiety, and depressive disorders. Alcohol health and research world. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6876499/#:~:text=The%20greater%20the%20amounts%20of,also%20are%20likely%20to%20intensify
Stöppler, M. (n.d.). Panic attack symptoms: Shortness of breath, racing heart, & more. WebMD. https://www.webmd.com/anxiety-panic/panic-attack-symptoms